
CHCS
Center for
Health Care Strategies, Inc.
Health Literacy
Implications of the
Affordable Care Act
Commissioned by:
The Institute of Medicine
Authored by:
Stephen A. Somers, PhD
Roopa Mahadevan, MA
Center for Health Care Strategies, Inc.
November 2010

Health Literacy Implications of the Affordable Care Act
© 2010 Center for Health Care Strategies, Inc.
S.A. Somers and R. Mahadevan. Health Literacy Implications of the Affordable Care Act. Center for Health Care Strategies, Inc.,
November 2010.
Contents
Acknowledgements ....................................................................................................................................... 3
I. Health Literacy and Health Care Reform ................................................................................................. 4
Health Literacy Until Now ...................................................................................................................... 5
II. Health Literacy and the Affordable Care Act ......................................................................................... 7
Definition ................................................................................................................................................. 7
Direct Mentions ....................................................................................................................................... 7
Indirect Provisions ................................................................................................................................... 9
Insurance Reform, Outreach, and Enrollment ................................................................................ 9
Individual Protections, Equity, and Special Populations .............................................................. 11
Workforce Development ............................................................................................................... 13
Health Information ........................................................................................................................ 14
Public Health, Health Promotion, and Prevention & Wellness ................................................... 16
Innovations in Quality and the Delivery and Costs of Care ......................................................... 18
Best Practices: “What Are My Medi-Cal Choices?” .............................................................................. 20
III. Conclusion ............................................................................................................................................ 21
IV. Appendices ........................................................................................................................................... 22
Appendix A: Summary of ACA Provisions with Potential Implications for Health Literacy ............. 22
Appendix B: Instances of “Culturally and Linguistically Appropriate” in the ACA .......................... 31
The Center for Health Care Strategies (CHCS) is a nonprofit health policy resource center dedicated to improving health
care quality for low-income children and adults, people with chronic illnesses and disabilities, frail elders, and racially and
ethnically diverse populations experiencing disparities in care. CHCS works with state and federal agencies, health plans,
providers and consumer groups to develop innovative programs that better serve Medicaid beneficiaries with complex and
high-cost health care needs. Its program priorities are: improving quality and reducing racial and ethnic disparities; integrating
care for people with complex and special needs; and building Medicaid leadership and capacity.

Health Literacy Implications of the Affordable Care Act
3
Acknowledgements
he authors thank Sara Rosenbaum, Hirsh Professor and Chair of Health Policy at George
Washington University, for her cogent analysis of the legislation and insights into the opportunities
it presents for promoting health literacy. We also wish to acknowledge the contributions of our
colleagues at Center for Health Care Strategies (CHCS), particularly Stacey Chazin, Michael Canonico,
Vincent Finlay, and Dorothy Lawrence, for their assistance in preparing this document.
CHCS expresses appreciation to the Institute of Medicine (IOM) for commissioning this report,
highlights of which the authors shared at the IOM Health Literacy Roundtable Workshop in
Washington D.C., on November 10, 2010.
T

Health Literacy Implications of the Affordable Care Act
4
I. Health Literacy and Health Care Reform
lthough low health literacy is certainly not a featured concern of the health care reform legislation
passed in early 2010, there are those who would argue that the law cannot be successful without a
redoubling of national efforts to address the issue. Nearly 36 percent of America’s adult population — 87
million adults — is considered functionally illiterate.
1
As the Patient Protection and Affordable Care
Act (ACA) extends health insurance coverage to some 32 million lower-income adults and promotes
greater attention to the barriers faced by individual patients, those implementing the law should consider
how to incorporate health literacy into strategies for enrolling beneficiaries and delivering care.
For the purposes of this paper, health literacy is defined, using the National Library of Medicine’s
definition, as:“The degree to which individuals have the capacity to obtain, process, and understand basic health
information and services needed to make appropriate health decisions.”
2
Fortunately, several ACA provisions directly acknowledge the need for greater attention to health
literacy, and many others imply it. The law includes provisions to communicate health and health care
information clearly; promote prevention; be patient-centered and create medical or health homes; assure
equity and cultural competence; and deliver high-quality care. This paper identifies both the direct and
indirect links, and provides those concerned about health literacy with provision-specific opportunities
to support advancements. These provisions fall into six health and health care domains in the legislation
where further action may be called for by concerned stakeholders:
(1) Coverage expansion: enrolling, reaching out to, and delivering care to health insurance coverage
expansion populations in 2014 and beyond;
(2) Equity: assuring equity in health and health care for all communities and populations;
(3) Workforce: training providers on cultural competency, language, and literacy issues
(4) Patient information at appropriate reading levels;
(5) Public health and wellness; and
(6) Quality improvement: innovation to create more effective and efficient models of care,
particularly for those with chronic illnesses requiring extensive self-management.
Individuals with low levels of health literacy are least equipped to benefit from the ACA, with
potentially costly consequences for both those who pay for and deliver their care, as well as for
themselves. Rates of low literacy are disproportionately high among lower-income Americans eligible for
publicly financed care through Medicare or Medicaid.
3
In 2014, this pattern is likely to extend to
individuals newly eligible for Medicaid or for publicly subsidized private insurance through state-based
exchanges.
1
J. Vernon, A. Trujillo, S. Rosenbaum, and B. DeBuono. Low Health Literacy: Implications for National Health Policy. University of
Connecticut, 2007.
2
S.C. Ratzan and R.M. Parker. Introduction. In: National Library of Medicine Current Bibliographies in Medicine: Health Literacy.
NLM Pub. No. CBM 2000-1 (2000).
3
M. Kutner et al. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy. U.S.
Department of Education, National Center for Education. Washington DC, 2006.
A

Health Literacy Implications of the Affordable Care Act
5
Health Literacy Until Now
In its Healthy People 2010 aims statement, the Department of Health and Human Services (HHS)
adopted the definition from the National Library of Medicine, declaring health literacy to be an
important national health priority. Healthy People 2010 broadened this definition to note that health
literacy is not just the problem of the individual, but also a by-product of system-level contributions.
4
Acknowledging the salience of this issue, HHS Secretary Kathleen Sebelius made official a federal
commitment to health literacy by releasing in May 2010 the National Action Plan to Improve Health
Literacy.
5
The plan lays out seven goals that emphasize the importance of creating health and safety
information that is accurate, accessible and actionable. It addresses payers, the media, government
agencies, health care professionals and others, recognizing the multi-sector effort that will be required to
effectively tackle this oft-ignored, national problem.
The U.S. health care system, with its myriad public and private programs, institutions, services, products,
and information, poses a significant challenge to those seeking access to affordable, quality health care.
Understanding the complexities of insurance eligibility, therapeutic guidance, medical technology,
prescription medication, disease management, prevention, and lifestyle modification are difficult for any
consumer, let alone one with compromised levels of literacy or numeracy (or quantitative literacy). An
individual seeking to participate successfully in the health system requires a constellation of skills —
reading, writing, basic mathematical calculations, speaking, listening, networking, and rhetoric — the
totality of which defines health literacy.
However, national data suggest that only 12 percent of adults have proficient health literacy.
6
While low
health literacy is found across all demographic groups, it disproportionately affects non-white racial and
ethnic groups; the elderly; individuals with lower socioeconomic status and education; people with
physical and mental disabilities; those with low English proficiency (LEP); and non-native speakers of
English.
7
Low health literacy is associated with reduced use of preventive services and management of
chronic conditions, and higher mortality.
8
It also leads to medication errors, misdiagnosis due to poor
communication between providers and patients, low rates of guidance and treatment compliance,
hospital readmissions, unnecessary emergency room visits, longer hospital stays, fragmented access to
care, and poor responsiveness to public health emergencies.
9
Accordingly, low health literacy has been
estimated to cost the U.S. economy between $106 billion and $236 billion annually.
10
The consequences of low health literacy have been recognized by federal agencies such as the Agency for
Healthcare Research and Quality (AHRQ), the Centers for Disease Control and Prevention (CDC), the
Food and Drug Administration (FDA), the Office of the Surgeon General, and the National Institutes of
Health (NIH), as well as by private organizations such as America’s Health Insurance Plans, the
American College of Physicians, the American Medical Association, The Joint Commission on
Accreditation, Kaiser Permanente, and Pfizer. These entities and many others are promoting awareness,
creating program initiatives, funding targeted research, setting readability standards, working with e-
health and social media platforms, and providing tools and resources for measurement and quality
4
R. Rudd. Objective 11-2. Improvement of Health Literacy. In: Communicating Health: Priorities and Strategies for Progress.
Office of Disease Prevention and Health Promotion, U.S. Department of Health and Human Services, Washington DC, 2003.
5
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. National Action Plan to
Improve Health Literacy. Washington DC, 2010.
6
National Center for Education Statistics, U.S. Department of Education. “2003 National Assessment of Adult Literacy (NAAL).”
Available at http://nces.ed.gov/naal/.
7
L. Neilsen-Bohlman, A.M. Panzer, and D.A. Kindig. Health Literacy: A Prescription to End Confusion. National Academies Press.
Washington DC, 2004.
8
N.D. Berkman, et al. Literacy and Health Outcomes. Agency for Healthcare Research and Quality (AHRQ). Rockville, MD, 2004.
9
Neilsen-Bohlman et al, op cit; Berkman et al, op cit., Vernon et al, op cit.
10
Vernon, et al., op cit.

Health Literacy Implications of the Affordable Care Act
6
improvement across providers, health plans, hospitals, and employer organizations. Important policy
papers such as the Institute of Medicine’s (IOM) 2004 report, Health Literacy: A Prescription to End
Confusion,
11
and national data such as those produced by the National Adult Literacy Survey
12
have
contributed to the knowledge base for this issue.
To date, however, strong legislative language, regulations, and appropriations for concerted efforts to
address health literacy have not emerged from the federal government. Congressional bills such as the
National Health Literacy Act of 2007
13
and the Plain Language Act of 2009,
14
which mapped out
meaningful health literacy strategies, have not yet made it to the President’s desk. It remains to be seen
whether the ACA can be used to push the national health literacy agenda forward.
11
Neilsen-Bohlman, et al., op cit.
12
National Center for Education Statistics, op cit.
13
U.S. Congress. “S. 2424: National Health Literacy Act of 2007.” 110
th
Congress. 2007 – 2008. Available at: http://www.
govtrack.us/congress/bill.xpd?bill=s110-2424.
14
U.S. Congress. “H.R. 946: Plain Writing Act of 2010.” 111
th
Congress 2009 – 2010. Available at: http://www.govtrack.us/
congress/bill.xpd?bill=h111-946. Note: The Plain Language Act of 2009 was mooted by passage of a related bill, the Plain
Writing Act of 2010, which was signed into law by President Obama on October 13, 2010, following completion of this paper.

Health Literacy Implications of the Affordable Care Act
7
II. Health Literacy and the Affordable Care Act
he ACA is, by any measure, a major piece of domestic policy legislation, directly affecting tens of
millions of Americans at a cost of nearly one trillion dollars over the next 10 years. The law’s
primary goals are to increase access to coverage, regulate the private insurance industry to allow more
Americans into the system at affordable rates, and begin to control the rate of growth in health care
costs. These goals cannot be achieved, however, without efforts to address cultural, linguistic and social
barriers to care facing vulnerable populations. Low health literacy is critical among these barriers. The
following ACA provisions include direct and indirect language concerning health literacy:
Definition
Title V, Subtitle A (amending existing laws and creating new law related to the health care workforce)
of ACA establishes a statutory definition of “health literacy” consistent with Healthy People 2010. The
term is defined as “the degree to which an individual has the capacity to obtain, communicate, process,
and understand health information and services in order to make appropriate health decisions.” Other
direct mentions of health literacy do not specifically cross-reference the Title V definition (though
presumably, HHS will use this terminology when implementing the various titles of the law).
Direct Mentions
Table 1 contains the law’s four other direct mentions of the term health literacy, These provisions touch
on issues of research dissemination, shared decision-making, medication labeling, and workforce
development. All four suggest the need to communicate effectively with consumers, patients, and
communities in order to improve the access to and quality of health care. None of these provisions
creates explicit health literacy programs, specifies implementation or regulatory supports, or expounds
further on the term “health literacy” beyond its mention. However, they are all consistent with the
themes of patient-centeredness and overall quality improvement that are found more broadly throughout
the legislation.
T
Health Literacy Implications of the Affordable Care Act
8
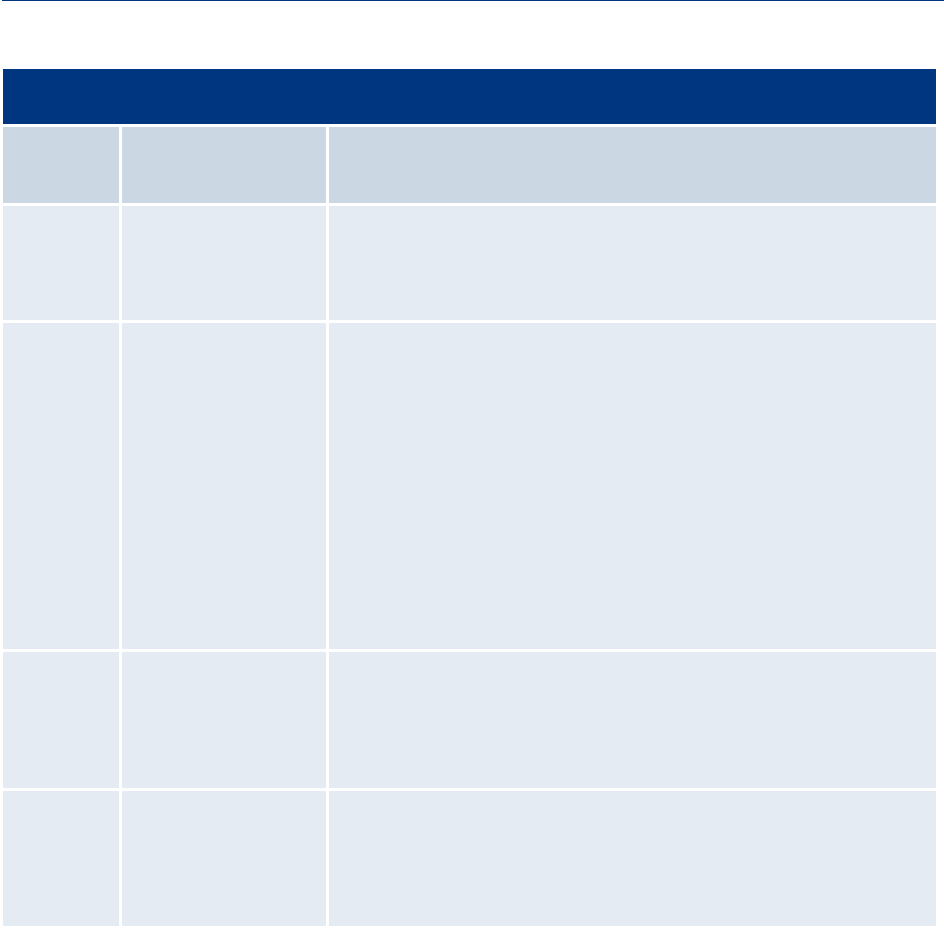
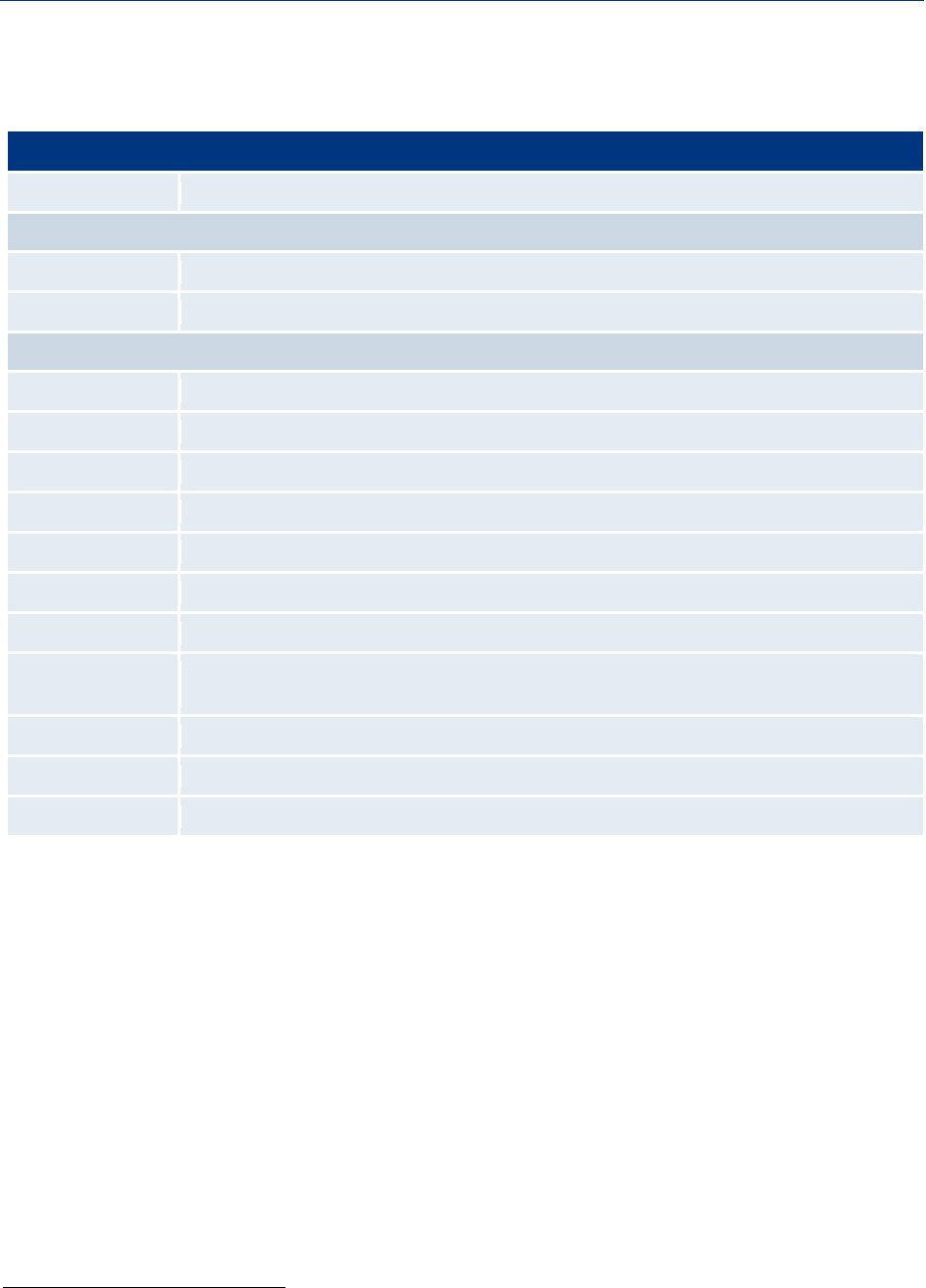
TABLE 1: ACA Provisions with Direct References to “Health Literacy”
Section
Number
Provision Title Legislative Language
Sec. 3501 Health Care Delivery
System Research;
Quality Improvement
Technical Assistance
Requires that research of the AHRQ’s Center for Quality Improvement and
Patient Safety be made “available to the public through multiple media and
appropriate formats to reflect the varying needs of health care providers and
consumers and diverse levels of health literacy.”
Sec. 3506 Program to Facilitate
Shared Decision-
making
Amends the Public Health Service Act to “facilitate collaborative processes
between patients, caregivers, authorized representatives and clinicians that
enables decision-making, provides information about tradeoffs among
treatment options, and facilitates the incorporation of patient preferences and
values into the medical plan.”
Authorizes a “program to update patient decision aids to assist health care
providers and patients.” The program, administered by the CDC and NIH,
awards grants and contracts to develop, update, and produce patient decision
aids for preference-sensitive care to assist providers in educating patients,
caregivers, and authorized representatives concerning the relative safety,
effectiveness and cost of treatment, or where appropriate, palliative care.
“Decision aids must reflect varying needs of consumers and diverse levels of
health literacy.”
Sec. 3507 Presentation of
Prescription Drug
Benefit and Risk
Information
Directs the Secretary to determine whether the addition of certain standardized
information to prescription drug labeling and print advertising would improve
health care decision-making by clinicians and patients and consumers; to
consider scientific evidence on decision-making; and to consult with various
stakeholders and “experts in health literacy.”
Sec. 5301
Training in Family
Medicine, General
Internal Medicine,
General Pediatrics, and
Physician Assistantship
Amends Title VII of the Public Health Service Act to permit the Secretary to
make training grants in the primary care medical specialties. Preference for
awards are for qualified applicants that “provide training in enhanced
communication with patients. . . and in cultural competence and health
literacy.”
Health Literacy Implications of the Affordable Care Act
9
Indirect Provisions
Other instances where the concept of health literacy could come into play include those discussed in the
following sections, organized into the six domains introduced at the outset. See the appendices for an
extensive list and descriptions of these and other provisions.
Insurance Reform, Outreach, and Enrollment
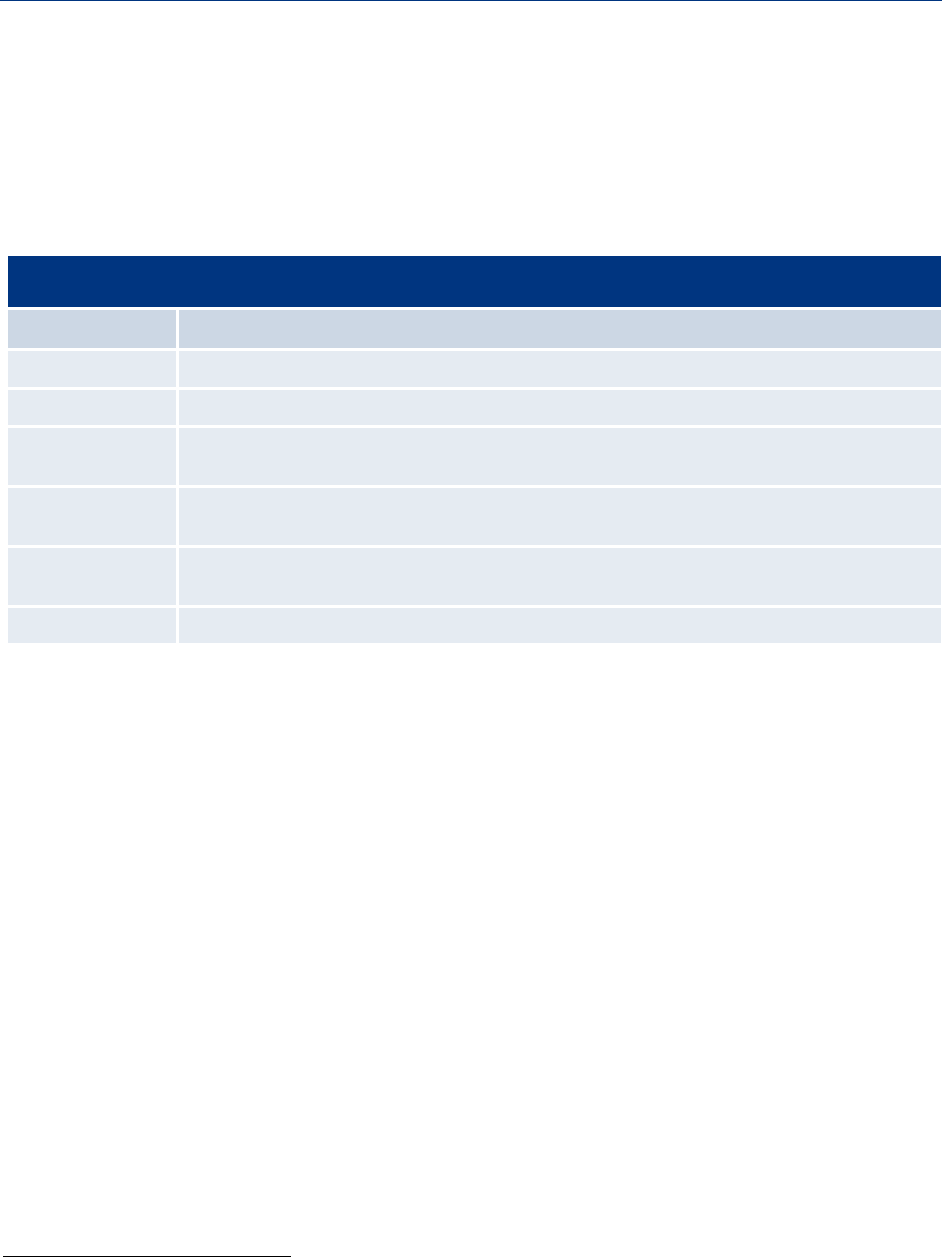
TABLE 2: Provisions Related to Insurance Reform, Outreach, and Enrollment
Section Number Provision Title
Sec. 1002 Health insurance consumer informatio
n
Sec. 1103 Immediate information that allows consumers to identify affordable coverage options
Sec. 1311 Affordable choices of health benefit plans
(includes language on “culturally and linguistically appropriate” obligations for plans)
Sec. 1413 Streamlining of procedures for enrollment through an Exchange and State Medicaid, CHIP, and
health subsidy programs
Sec. 2715 Development and utilization of uniform explanation of coverage documents and standardized
definitions.
Sec. 3306 Funding outreach and assistance for low-income programs.
Health insurance market reforms have substantial potential for reducing inequities in the health system
that are interrelated with insurance status. For example, the National Assessment of Adult Literacy
found that adults with no insurance are more likely to have “basic” or “below basic” health literacy than
“intermediate” or “proficient” health literacy.
15
A literature review prepared for the Kaiser Family
Foundation revealed that health insurance is the single-most significant factor explaining racial
disparities in having a usual source of care.
16,17
Broadly speaking, the ACA intends to improve access to health insurance in four main ways: (1) the
individual mandate, which requires all persons to have “qualifying or acceptable coverage”; (2) employer
mandates requiring coverage for employees in businesses with more than 50 employees; (3) regional/state
exchanges that allow individuals and small businesses to purchase coverage of varying benefit and cost,
and choose from subsidized plans (for those up to the 400 percent of the federal poverty level, or FPL);
and 4) the expansion of Medicaid eligibility to all individuals up to 133 percent of FPL. Additional
provisions seek to broaden the scope and affordability of insurance coverage by, among other things:
prohibiting insurance companies from rescinding coverage; extending dependent coverage for young
adults until age 26; eliminating lifetime limits on coverage; regulating annual dollar limits on insurance
coverage; and prohibiting the denial of coverage to children based on pre-existing conditions.
As many of those charged with implementing the ACA realize, none of these reforms will fully succeed
without efforts to make all of these opportunities understandable to the intended beneficiaries. These
expansions must be accompanied by targeted efforts to enroll under-resourced populations. Given their
15
National Center for Education Statistics, op cit.
16
Testimony of M. Lillie-Blanton, Dr.P.H., Senior Advisor on Race, Ethnicity, and Health Care, Henry J. Kaiser Family Foundation,
before the House Ways and Means Subcommittee on Health. June 10, 2008.
17
American College of Physicians. Racial and Ethnic Disparities in Health Care, Updated 2010. Philadelphia: American College of
Physicians, 2010.

Health Literacy Implications of the Affordable Care Act
10
inexperience with health coverage and the delivery system, these individuals will have greater difficulty
with a number of its facets: understanding eligibility guidelines for various insurance programs;
participating in the buy-in process of the exchange or high-risk pools; providing supplemental
identification and citizenship documentation necessary for enrollment; understanding which services are
covered; recognizing cost-sharing and premium responsibilities; and choosing a health care provider. All
of these tasks require significant consumer education and assistance. Notably, one ACA provision calls
for the development and utilization of uniform explanations of coverage documents and standardized
definitions. This is an important mandate that could be strengthened with explicit linkages to health
literacy.
The ACA also establishes an internet portal to help individuals and businesses interact with the
insurance exchange. This tool will have to assist users in understanding eligibility guidelines for
Medicaid/CHIP/Medicare/high-risk pools and subsidized private insurance. As such, the portal should
contain easy-to-understand explanations in simple English, as well as be available in multiple languages.
The ACA also requires that information presented by the national and regional exchanges be culturally
and linguistically appropriate.
To be most effective, ACA requirements to make insurance and enrollment information consumer-
friendly should extend beyond readable web and print materials to include media such as phone,
television, radio, social media, and in-person outreach. Research shows that a higher percentage of adults
with low literacy receive their information about health issues from radio and television than through
written sources, the internet, or social contacts.
18
Use of community-based organizations, culturally
specific media campaigns, promotores, and individual insurance brokers (many of whom will be displaced
due to the exchanges) will drive effective enrollment of the highly diverse, newly eligible population.
The economic recession has shown, for example, that affected families have turned first to community-
based organizations for help with linking them to public assistance programs.
19
States can use specially
allocated ACA funding for such local outreach and enrollment supports.
Medicaid Expansion. ACA law mandates that starting in 2014, Medicaid cover everyone under age 65
and 133 percent of FPL ($14,404 for one person in 2009). Accordingly, Medicaid could be serving
upwards of 80 million Americans — or a quarter of the U.S. population — each year after 2014. Recent
analyses suggest that this “expansion population” will likely: be racially and ethnically diverse; be
predominantly childless adults; have high levels of substance abuse and prior jail involvement; and
require integrated care management for complex physical and behavioral health needs.
20
It is fair to
assume that health literacy would be a significant issue for this population, as current Medicaid
beneficiaries face serious communication barriers related to limited literacy, language, culture, and
disability.
21
Most new enrollees are unlikely to have had prior insurance, and thus will have limited
knowledge about the Medicaid program, its services, and the complex administrative processes associated
with enrollment and participation.
Simplifying Medicaid enrollment for diverse populations is not a new concept: the majority of states
have some health literacy standards for their Medicaid programs. About 90 percent of all states have
18
M. Kutner, et al. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy.
Washington, DC: U.S. Department of Education, National Center for Education, 2006.
19
Kaiser Commission on Medicaid and the Uninsured. Optimizing Medicaid Enrollment: Perspectives on Strengthening Medicaid’s
Reach under Health Care Reform. Kaiser Family Foundation, Publication #8068, April 2010.
20
S. A. Somers, A. Hamblin, J. Verdier and V. Byrd. Covering Low-Income Childless Adults in Medicaid: Experiences from Selected
States. Center for Health Care Strategies. August 2010.
21
L. Neuhauser B. Rothschild, C. Graham, S.L. Ivey and S. Konishi. “Participatory Design of Mass Health Communication in Three
Languages for Seniors and People with Disabilities on Medicaid.” American Journal of Public Health (2009), 99(12): 2188-2195.

Health Literacy Implications of the Affordable Care Act
11
specific readability guidelines for Medicaid enrollment materials.
22
Of these, 67 percent call for at least a
sixth-grade reading level or a range including, and 22 percent call for the level to be even lower. Ninety-
six percent of states have simplified their enrollment forms, using easy-to-read language and repetition of
key messages, such as when to use emergency care services. Eighty-two percent of states offer one-on-one
enrollment assistance, and 72 percent provide onsite assistance at state agency offices, counseling
sessions at local nonprofits and community centers, and/or a toll-free helpline.
23
Despite these efforts,
many racial and ethnic minorities eligible for Medicaid or CHIP coverage — more than 80 percent of
eligible uninsured African-American children and 70 percent of eligible uninsured Latino children —
are still not enrolled.
24
For current Medicaid beneficiaries who do not speak English or who have LEP, most states provide
interpretive and translation services. The Centers for Medicare and Medicaid Services (CMS) has
released readability guidelines for Medicaid print materials to states and has mandated certain contract
requirements around communication standards for Medicaid managed care plans.
25
However, these
guidelines lack strong enforcement or uniform oversight from any particular federal or state agency.
The following three ACA provisions, while not clearly linked to literacy, help further to simplify
Medicaid eligibility determinations and streamline enrollment: (1) elimination of the asset test that
many states still apply when determining Medicaid eligibility for adults, removing a common
administrative burden and impediment to participation; (2) usage of a new, uniform method for
determining income eligibility for most individuals (modified adjusted gross income, or MAGI); and (3)
the expansion of the state option to presumptive eligibility determinations. The ACA also streamlines
citizenship documentation requirements and electronic enrollment processes set forth by the Children’s
Health Insurance Program Reauthorization (CHIPRA) legislation in 2009.
26
To the extent that federal
entities could provide monetary and technical assistance support for state health literacy efforts,
Medicaid programs would be better able to effectively enroll and provide quality care to newly eligible,
low-literacy populations in 2014 and beyond.
Individual Protections, Equity, and Special Populations
TABLE 3: Provisions Related to Individual Protections, Equity, and Special Populations
Sample of Indirect Instances where Health Literacy could be addressed
Section Number Provision Title
Sec. 1557. Nondiscrimination
Sec. 4302. Understanding health disparities; data collection and analysis
Sec. 6301. Patient-centered outcomes research
Sec. 10334. Minority health
The Insurance expansions in the ACA constitute significant steps toward universal coverage. All
Americans up to a certain level of poverty (133 percent) will for the first time be entitled to health
22
Health Literacy Innovations, LLC. National Survey of Medicaid Guidelines for Health Literacy. 2003.
23
T. Matthews and J. Sewell. State Official's Guide to Health Literacy. Lexington, KY: Council of State Governments, 2002.
24
American College of Physicians, op cit.
25
Rosenbaum et al. The Legality of Collecting and Disclosing Patient Race and Ethnicity Data. George Washington University
Department of Health Policy, 2006.
26
U.S. Congress. “H.R. 2: Children’s Health Insurance Program Reauthorization Act of 2009.” Available at: http://www.
govtrack.us/congress/bill.xpd?bill=h111-2.

Health Literacy Implications of the Affordable Care Act
12
insurance. Protecting these lower-income individuals’ right to health care is important to the successful
implementation of the ACA. The law references the Civil Rights Act, the Education Amendments Act,
the Age Discrimination Act, and the Rehabilitation Act. Section 1557’s Non-Discrimination provision
prevents exclusion of an individual from participation in or denial of benefits under any health program
or activity.
The ACA also provides consumers with significant new protections, including the ability to choose a
health plan that best suits their needs, to appeal a plan’s denial of coverage for needed services, and to
select an available primary care provider of their choosing. Health plans are now required to
communicate these patient protections in media that are “culturally and linguistically appropriate,” and
by extension, readable for those with low literacy levels. This term is used seven times in the legislation,
including in references to: federal oral health and nutrition education programs; clinical depression
centers of excellence; workforce training curricula; and the need for patient-centered delivery models to
be culturally competent, i.e. sensitive to the beliefs, values, and cultural mores that influence how health
care information is shared and received by individuals. Prior efforts of the HHS’ Office of Civil Rights to
set compliance standards for language aimed to improve access for those who have LEP and are already
providing related regulations. But, there is no language in the ACA instructing this body or others to
oversee the new “culturally and linguistically appropriate” obligations.
ACA law also requires the collection and reporting of data on race, ethnicity, sex, primary language, and
disability status by all federally conducted and supported health care and public health programs (e.g.,
Medicare, Medicaid), activities, and surveys (including surveys conducted by the Bureau of Labor
Statistics and the Bureau of the Census). It also urges the HHS to strengthen existing requirements that
state Medicaid agencies collect race, ethnicity, and language data. The law specifies that existing Office
of Management and Budget standards must be used, at a minimum, for recording race and ethnicity, and
instructs the HHS to issue new standards for measuring sex, primary language, and disability status.
In 2000, the Office of Minority Health (OMH) developed National Standards on Culturally and
Linguistically Appropriate Services (CLAS) to provide a common understanding and consistent
definitions of culturally and linguistically appropriate services in health care. These standards were
intended to be a practical framework for providers, payers, accreditation organizations, policymakers,
health administrators, and educators. Post-reform health literacy efforts should make use of this resource,
particularly since the OMH is gaining additional recognition in the law. The ACA establishes an OMH
in every major agency within the HHS: AHRQ, CDC, CMS, FDA, Health Resources and Services
Administration (HRSA), and Substance Abuse and Mental Health Services Administration
(SAMHSA). These offices will be charged with evaluating the effectiveness of federal programs and
targeted research to meet the needs of minority populations. Similarly, a newly created Patient Centered
Outcomes Research Institute is tasked with conducting comparative effectiveness research, and ensuring
that subpopulations, particularly communities of color, are represented in research designs.
The ACA’s disparities agenda includes additional measures to support the rights and unique needs of
certain populations. These include standardizing complaint forms for patients in nursing facilities;
improving quality of care and protections for those in long-term care institutions; expanding aging and
disability resource centers; providing dementia prevention and abuse training for personnel working in
geriatric mental health; supporting pregnant and parenting teens and women through health care, social,
and educational assistance; and appropriating funds for the Indian Health Care Improvement Act,
27
which supports the growth of the Native American health care force and innovative delivery models for
27
U.S. Congress. “S.1790: Indian Health Care Improvement Reauthorization and Extension Act of 2009.” Dorgan, B. Available at:
http://www.govtrack.us/congress/bill.xpd?bill=s111-1790.
Health Literacy Implications of the Affordable Care Act
13
rural populations and tribal organizations. Again, however, these provisions make no explicit link to
health literacy.
Workforce Development
TABLE 4: Provisions Related to Workforce Development
Section Number Provision Title
Direct Mentions of Health Literacy
Sec. 5301 Training in family medicine, general internal medicine, general pediatrics, and physician assistantship
Sample of Indirect Instances where Health Literacy could be addressed
Sec. 5205 Allied health workforce recruitment and retention program
Sec. 5307 Cultural competency, prevention, and public health and individuals with disabilities training
Sec. 5313 Grants to promote the community health workforce
Sec. 5402 Health professions training for diversity
Sec. 5403 Interdisciplinary, community-based linkages
Sec. 5507
Demonstration project to address health professions workforce needs; extension of family-to-family
health information centers
Sec. 5606 State grants to health care providers who provide services to a high percentage of medically
underserved populations or other special populations
Within the next 40 years, people of color will make up the majority of the U.S. population.
28
Insurance
reforms and expansion of coverage will bring to providers’ offices new socially, culturally, and
linguistically diverse patient populations, many of which are likely to have limited experience with the
health system, difficulty communicating with practitioners, and complex conditions that require
effective self-management. There will be increased onus on health care providers and their delivery
system partners to be sensitive to the nuanced needs and potential limitations of their patient
populations. Not doing so could have major consequences for the patient’s health, the physician’s
performance, and the payer’s pocketbook.
Effectively communicating with low-literate patients is not an arcane skill: a survey of Federally
Qualified Health Centers, free clinics, and migrant health facilities found that when clinicians use plain
language, illustrations, and “talk back” methods, patient understanding, compliance, and trust are greatly
improved.
29
As it stands today, however, physicians are given little training in this area during the course
of their medical education,
30
and professionals who do receive a modicum of training in this vein —
community health workers and nurses, case managers, and public health specialists, for example — lack
recognition, funding, and inclusion in most physician-led delivery teams. Other system issues such as
pressure on provider time, use of singular modes of communication, and cultural mismatch between
provider and patient also contribute to subpar delivery of health care services to low-literate patients.
31
28
U.S. Census Bureau. “Projected Population of the United States, by Race and Hispanic Origin: 2000 to 2050.” Available at:
http://www.census.gov/ipc/www/usinterimproj/natprojtab01a.pdf.
29
Barrett S.E et al. Health Literacy Practices in Primary Care Settings: Examples from the Field. The Commonwealth Fund, 2008.
30
American College of Physicians. Racial and Ethnic Disparities in Health Care, Updated 2010. Philadelphia: American College of
Physicians, 2010.
31
M.K. Paasche-Orlow, D. Schillinger, S.M. Green, and E.H. Wagner. “How Healthcare Systems can Begin to Address the
challenge of Limited Literacy. Journal of General Internal Medicine, 21(8): 884–887 (2006).

Health Literacy Implications of the Affordable Care Act
14
Appropriately, the ACA legislation pushes for improvement in the education and communications skills
of a wide range of health provider types, positioning workforce development as an important lever for
establishing health care equity across diverse patient populations.
The ACA provides scholarships, grants, and loan repayment programs for health care professionals in
medical fields such as primary care and mental health; offers continuing education support for those who
serve minority, rural, and special populations; and improves medical school and health professions
curricula in the areas of cultural competency and disabilities training. The ACA also seeks to increase
the racial/ethnic diversity of health practitioners through educational grants and loan programs, and
widens the array of professional and para-professionals available to patients through funding for training
of community health workers, nurses, geriatric specialists, adolescent mental health providers, home care
aides, and others.
Only one of these provisions — the primary care provider workforce training awards — explicitly
mentions the term health literacy. But, other language related to cultural and linguistic appropriateness
appears frequently, particularly as a condition of eligibility for the workforce grant opportunities.
Health Information
TABLE 5: Provisions Related to Health Information
Section Number Provision Title
Direct Mentions of Health Literacy
Sec. 3507 Presentation of prescription drug benefit and risk information
Sample of Indirect Instances where Health Literacy could be addressed
Sec. 3305 Improved information for subsidy eligible individuals reassigned to prescription drug and
MA-PD Plans
Sec. 3503 Grants to implement medication management services in treatment of chronic disease
Sec. 4205
N
utrition labeling of standard menu items at chain restaurants
Sec. 10328 Improvement in Part D medication therapy management (MTM) programs
While the average piece of health care information is written at a 10th-grade reading level, the average
American reads at only a fifth-grade level.
32
Numerous studies show that those with limited health
literacy skills are at increased risk of misunderstanding medical information on product labels, manuals,
package inserts, and nutrition labels.
33
,
34
The ACA provisions on nutrition labeling, the presentation of prescription drug information, and
medical management assistance are welcome. These provisions do not mandate health system-wide
standards but recommend small-scale changes and building an evidence base for future implementation.
They constitute an important step in acknowledging that health information, which is often dense,
technical, and jargon-filled, must be digestible to the diverse consumers who are trying to use it.
32
Rosales. “Are Adequate Steps Being Taken to Address Health Literacy in this Country?” Managed Care Outlook, 23(11), June 1,
2010.
33
Institute of Medicine. Preventing Medication Errors: The Quality Chasm Series. National Academies Press, 2006.
34
B.D. Weiss, M.Z. Mays, et al, “Quick Assessment of Literacy in Primary Care: The Newest Vital Sign.” Annals of Family Medicine
(2005), 3:514-522.

Health Literacy Implications of the Affordable Care Act
15
For example, due to the high national prevalence of cardio-metabolic conditions, consumers have a
greater need to read and interpret labels that provide information on sugar, fat, salt, and cholesterol
content. Difficulties in understanding nutrition information are heightened for those with “basic” and
“below basic” levels of literacy.
35
These individuals have trouble finding pieces of information or numbers
in a lengthy text, integrating multiple pieces of information in a document, or finding two or more
numbers in a chart and performing a calculation.
36
Elders and others with multiple chronic conditions are often given prescriptions for numerous
medications by a mix of physical health and mental health providers, who may not communicate with
each other about their prescription practices. This places the onus of medication reconciliation on the
patient, whose literacy and numeracy skills might be compromised.
Complications around choice of plan eligibility and prescription drug reimbursement add other
challenges for Part D Medicare beneficiaries. ACA provisions call for improved information for subsidy-
eligible individuals reassigned to prescription drug and MA-PD plans, and put into place medication
management programs for Part D seniors and chronic disease patients. These should help vulnerable
beneficiaries with their health information demands. To be effective, these efforts should also focus on
the verbal communications used by providers, pharmacists, and other dispensers of medication, to ensure
that patients understand medication dosage, schedules, side effects and safety precautions.
Given the increasing presence of information technology in health communications, delivery and
management, it will be important that this medium be accessible to low-literate, and low computer-
literate users in particular. In several instances, the ACA promotes the use of the internet and web-based
tools to disseminate health information and to communicate federal activities to a diverse consumer
population. Some of these include:
The “ombudsman” portal to facilitate enrollment into public and publicly subsidized insurance
programs and the exchange;
A website recommending prevention practices for specified chronic diseases and conditions;
A web-based tool to create personalized prevention plans; and
An internet portal for consumers to access health risk assessment tools.
Those designing these media should look to resources like the Health Literacy Online Guide,
37
a research-
based how-to module developed by the HHS’ Office of Disease Prevention and Health Promotion
(ODPHP) to guide administrators, providers, and educators seeking to present information to low-
literacy Americans using the web.
In terms of promoting the meaningful use of electronic health records (EHRs), there is little in the ACA
that speaks to health literacy. However, health literacy advocates might note relevant requirements in
the American Recovery and Reinvestment Act (ARRA)
38
legislation: (1) patients must be provided
timely access (within 96 hours) to their electronic health information; (2) the EHR should be used to
35
The Joint Commission. What did the Doctor Say?: Improving Health Literacy to Protect Patient Safety. Joint Commission, 2007
36
Berkman et al, op cit.
37
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Health Literacy Online: A
Guide to Writing and Designing Easy-to-Use Health Web Sites. Washington, D.C., 2010. Available at:
http://www.health.gov/healthliteracyonline/.
38
U.S. Congress. “H.R.1: American Recovery and Reinvestment Act of 2009.” Obey, D. Available at: http://www.govtrack.us/
congress/bill.xpd?bill=h111-1.
Health Literacy Implications of the Affordable Care Act
16
identify and provide patient-specific education resources; and (3) health care providers using an EHR
must collect race and ethnicity data on their patients, using the OMB’s classification standards.
Public Health, Health Promotion, and Prevention & Wellness
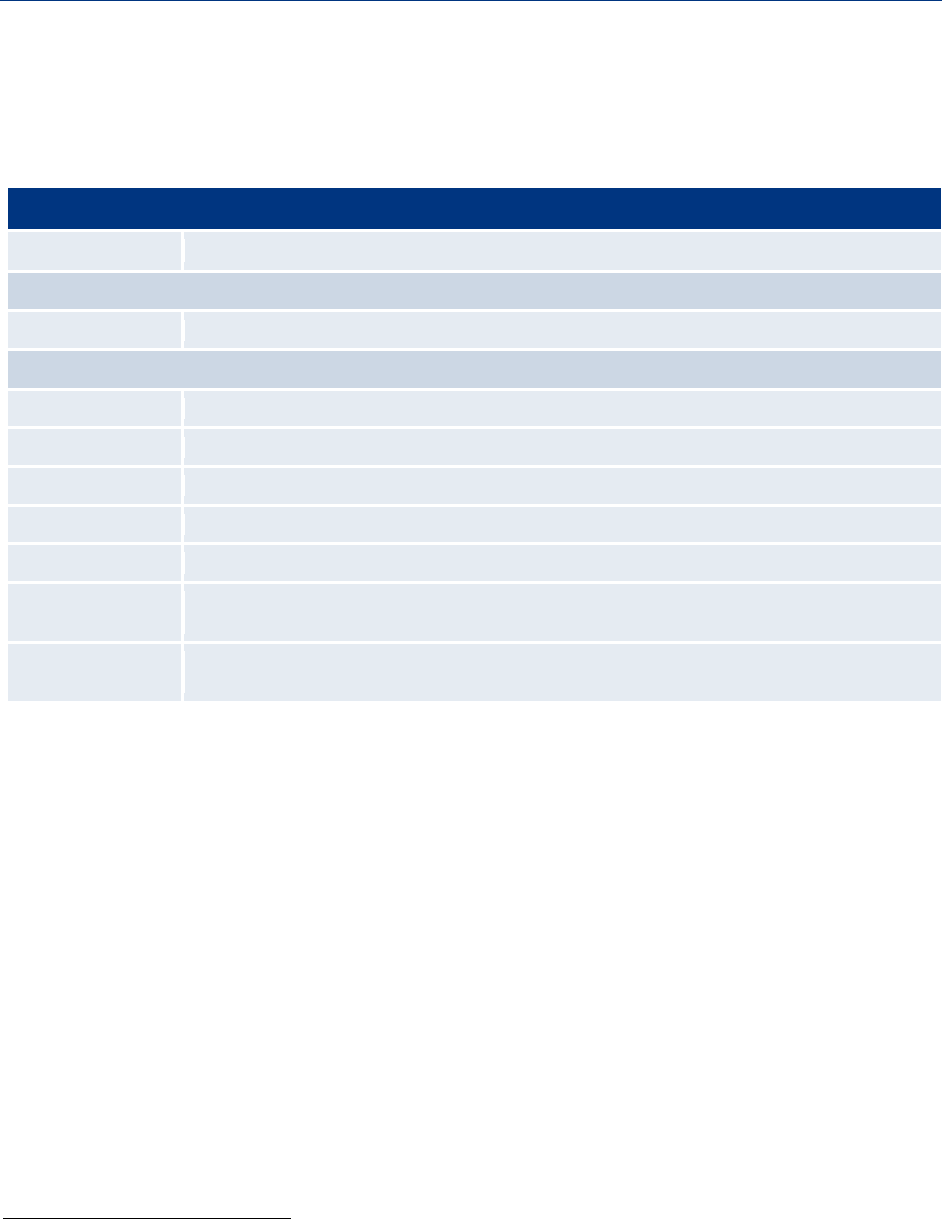
TABLE 6: Provisions Related to Public Health, Health Promotion, and Prevention & Wellness
Section Number Provision Title
Sec. 2951 Maternal, infant, and early childhood home visiting programs
Sec. 2953 Personal responsibility education
Sec. 4001
N
ational Prevention, Health Promotion and Public Health Council
Sec. 4002 Prevention and Public Health Fund
Sec. 4003 Clinical and Community Preventive Services
Sec. 4004 Education and outreach campaign regarding preventive benefits
Sec. 4102 Oral healthcare prevention
a
ctivities
Sec. 4103 Medicare coverage of annual wellness visit providing a personalized prevention plan
Sec. 4107 Coverage of comprehensive tobacco cessation services for pregnant women in Medicaid
Sec. 4108 Incentives for prevention of chronic diseases in Medicaid
Sec. 4201 Community transformation grants
Sec. 4202 Healthy Aging/Living Well for Medicare
Sec. 4206 Demonstration project concerning individualized wellness plan
Sec. 4303 CDC and employer-based wellness programs
Sec. 4306 Funding for childhood obesity demonstration project
Sec. 10408 Grants for small businesses to provide comprehensive workplace wellness programs
Sec. 10413 Young women’s breast health awareness and support of young women diagnosed with breast
cancer
Sec. 10501
N
ational diabetes prevention program
ACA establishes a comprehensive framework for federal, community-based public health activities,
including a coordinating council, a national strategy, and a national education and outreach campaign.
The legislation also addresses prevention and wellness at state, community, clinic, and organizational
levels. Specifically, it:
Expands coverage of clinical preventive services under Medicare, Medicaid, and private health
insurance;
Encourages the development and expansion of personalized wellness programs by employers and
insurers;

Health Literacy Implications of the Affordable Care Act
17
Expands federal grantmaking and other public health activities directed at the prevention of
disease risk factors such as obesity and tobacco use, with a focus on community transformation;
and
Supports evidence review processes to determine whether specific clinical (e.g. cancer
screenings) and community-based prevention interventions (e.g. media campaigns) are effective.
Notably, the large national outreach and education undertaking to be led by the HHS and CDC under
Sec. 4004 will include a science-based media campaign; a chronic disease website to educate consumers;
a web-based tool for individuals to create personalized prevention plans; and an internet portal with
health risk assessment tools developed by academic entities. In addition, each state must design a public
awareness campaign to educate Medicaid enrollees about the availability and coverage of preventive
services, such as obesity-reduction programs for children and adults. To be successful, these
communication efforts should include the use of multiple media streams to reach diverse populations.
ACA also requires Medicaid health plans to cover tobacco cessation counseling and drug therapy for
pregnant women. States that include a package of recommended preventive services (as set by the U.S.
Preventive Services Task Force) for Medicaid-eligible adults will receive an enhanced federal match.
Medicare Part B will be required to cover personalized prevention services for elders, including chronic
disease testing and treatment, medication reconciliation, cognitive impairment assessments, and tailored
wellness guidance. Other related programs authorized in the ACA that promote prevention and target
specific populations or health gap areas include: a national oral health education campaign; early
mother-child visiting programs; teenage personal responsibility grants; the pregnancy assistance fund; a
national diabetes prevention program; childhood obesity-reduction initiatives; and centers for excellence
in depression. These programs will address health literacy to the extent that they are attentive to issues
of information usability, consumer engagement and cultural competency.
Although competencies around emergency preparedness and infectious disease are not a notable part of
ACA’s public health provisions, they should not be ignored during the implementation of national and
community-based public health efforts. For example, individuals with compromised health literacy are
likely less equipped to receive pertinent information or act expeditiously in the face of environmental
disasters and pandemic disease outbreaks.
39
,
40
Being healthy or learning how to become and stay healthy requires substantial self-activation, resources,
willpower, and lifestyle modification. These are challenging for any patient, let alone one with low
health literacy, who may encounter other structural barriers to good health. Such obstacles may include
substandard housing; transportation difficulty; low job availability; poor educational opportunities;
higher exposure to environmental toxins; involvement with violence and criminal justice;
discrimination and socio-cultural marginalization; and limited access to fresh, healthy foods. These social
problems and the circumstances of “place” have been shown to have a significant impact on the health
of the underserved, many of whom also face low literacy.
41
,
42
39
C. Zarcadoolas, J. Boyer, A. Krishnaswami, and A. Rothenberg (2007). “How Usable are Current GIS Maps: Communicating
Emergency Preparedness to Vulnerable Populations?” Journal of Homeland Security and Emergency Management, 2007.
40
C. Zarcadoolas, A. Pleasant, and D.S.Greer. Advancing Health Literacy: A Framework for Understanding and Action. San
Francisco: Jossey-Bass, 2006.
41
B. Smedley. Building Stronger Communities for Better Health: Moving from Science to Policy to Practice. Presentation at IOM
Workshop, 2010.
42
Andrulis et al. Patient Protection and Affordable Care Act: Advancing Health Equity for Racially and Ethnically Diverse
Populations. Joint Center for Political and Economic Studies. Washington DC, July 2010.
Health Literacy Implications of the Affordable Care Act
18
Innovations in Quality and the Delivery and Costs of Care
TABLE 7: Provisions Related to Innovations in Quality and the Delivery and Costs of Care
Section Number Provision Title
Direct Mentions of Health Literacy
Sec. 3501 Health care delivery system research; quality improvement technical assistance
Sec. 3506 Program to facilitate shared decision-making
Sample of Indirect Instances where Health Literacy could be addressed
Sec. 2703 State option to provide health homes for enrollees with chronic conditions
Sec. 3011
N
ational strategy
Sec. 3012 Interagency Working Group on Health Care Quality
Sec. 3013 Quality measure development
Sec. 3014 Quality measurement
Sec. 3015 Data collection; public reporting
Sec. 3021 Establishment of Center for Medicare and Medicaid Innovation within CMS
Sec. 3502 Grants or contracts to establish community health teams to support the patient-centered
medical home
Sec. 3510 Patient navigator program
Sec. 10331 Public reporting of performance information
Sec. 10333 Community-based collaborative care networks
There is no dearth of provisions in the ACA focused on improving health care quality and reducing
avoidable costs. The legislation identifies patient-centeredness, safety, efficiency, and equity as both
vehicles for and by-products of the quality effort. Except for two mentions of health literacy in provisions
regarding shared decision-making programs and dissemination of delivery system research, health literacy
is not explicitly featured in the bill’s language on quality. However, adults with low health literacy
average six percent more hospital visits, remain in the hospital two days longer and have annual health
care costs four times higher than those with proficient health literacy skills.
43
As such, literacy should be
a core consideration in discussions of quality improvement, health delivery redesign, and cost-reduction.
The legislation uses three broad mechanisms to address quality: (1) a national approach that identifies an
umbrella strategy, establishes a federal-level, inter-agency quality workgroup, sets an agenda for
measurement, and develops metrics; (2) delivery system redesign through efforts targeting improved care
coordination and new patient-centered care models such as the medical home; and (3) the reduction of
cost through increased payer and provider accountability across private and public programs (e.g., pay-
for-performance incentives and value-based purchasing structures).
43
Partnership for Clear Health Communication at the National Patient Safety Foundation. What is Health Literacy? Ask Me 3.
Available at: http://www.npsf.org/askme3/PCHC/what_is_health.php.
Health Literacy Implications of the Affordable Care Act
19
Health literacy issues should ideally be represented in the ACA-mandated inter-agency quality
workgroup to be convened by the President, and in the development of the national quality strategy (i.e.,
readability standards for all federal health program communications). Quality measure development and
endorsement efforts that will be spearheaded by AHRQ and CMS should gauge national health literacy
trends and their implications, as well as explore how new measures that identify and stratify low-literacy
risk groups can be used to improve care at the community, provider, plan, and hospital levels. The
support for public reporting mechanisms in ACA may also provide consumers with better, more readable
information about the performance of their health system, enabling more informed health care choices.
Many of the objectives of quality improvement — avoiding waste in the system; reducing the over- and
underuse of medications, diagnostic tests, and therapies; and improving patient safety — depend on the
patient’s ability to be an informed and active player in his or her care. For low-literate populations,
interacting with physicians, complying with medical guidance, and managing the disparate demands of
multiple providers in fragmented delivery systems is that much more challenging.
Other ACA components that ensure patient-centeredness, such as the shared decision-making program
and patient navigator services, should also resonate with health literacy advocates. Regional
collaborative networks, primary care extension hubs, health homes in Medicaid, and community health
teams to support the medical home would all be strengthened by concerted attention to patients with
low literacy, particularly those managing complex, co-morbid physical and mental health conditions.
Estimates suggest that 75 percent of those with chronic conditions have low health literacy.
44
One of the most promising windows of opportunity among the quality-oriented provisions is the newly
created Center for Medicare and Medicaid Innovation (CMI) within CMS. CMI will fund
demonstration programs that research, test, and expand innovations in payment and delivery system
improvement pilots. Given the prevalence of low literacy among individuals in publicly financed care,
particularly people with disabilities in Medicaid and those dually eligible for Medicaid and Medicare,
45
this could be a prime opportunity to test health literacy innovations among high-risk populations such as
pregnant women or elders with multiple medications. Such demonstrations could convey to federal and
state policymakers the mediating power of health literacy to improve quality and reduce costs. This could
also help demonstrate the business case for further investments in health literacy by health plans and
accountable care organizations serving these populations.
Given the evidence base around populations disproportionately affected by low health literacy,
Medicaid, Medicare, and Veterans Administration programs may present the best targets of opportunity
for making the case. The Veterans Administration is a closed system with considerable data capacity, but
might pose problems for generalizability; while Medicare is still largely a fee-for-service system, which
provides few leverage points for concerted action. The 7.5 million individuals dually enrolled in
Medicaid and Medicare could benefit from health literacy interventions given their age and complex
health needs, but these “duals” are generally not in integrated care management programs that have
enormous incentives to prevent the exacerbation of illness and disability associated with low health
literacy. However, 71 percent of Medicaid’s 60 million beneficiaries are enrolled in managed care;
46
as the
nation’s largest purchaser of health care, Medicaid could use its leverage to promote innovations in this
arena. Medicaid managed care organizations already have the incentives to address health literacy,
especially for those with complex conditions. But, to date, none have demonstrated using readily
44
Hsu. The Health Literacy of U.S. Adults Across GED Credential Recipients, High School Graduates, and Non–High School
Graduates. American Council on Education. GED Testing Service, 2008.
45
Baker et. al. “Health Literacy and Mortality among Elderly Persons.” Archives of Internal Medicine (2007), 167(14):1503-1509.
46
Centers for Medicare and Medicaid Services, U.S. Department of Health and Human Services. “Medicaid Managed Care
Penetration Rates by State as of June 30, 2008.” Special data request, August 2009.
Health Literacy Implications of the Affordable Care Act
20
available and easy-to-administer literacy assessment tools (e.g., the short TOHFLA) to: 1) identify and
stratify a high-risk population with low literacy skills, and 2) design interventions to support health
management and consequently avoid costly exacerbations, hospitalizations and institutionalizations.
Best Practices: “What Are My Medi-Cal Choices?”
Health Research for Action (HRA), a center at UC Berkeley’s School of Public Health, was funded by the
California Department of Health Care Services (DHCS) to create easy-to-read and understandable
information for seniors and people with disabilities on Medi-Cal, about their Medi-Cal choices. This specific
population could choose between Regular Medi-Cal (also known as Fee for Service) and Medi-Cal Managed
Care Plans. The goals of this project were to:
1. Use participatory research to develop a guidebook that informed seniors and people with
disabilities on Medi-Cal about their unique Medi-Cal choices.
2. Promote informed choice between Medi-Cal fee for service and Medi-Cal Managed Care delivery
systems.
HRA conducted extensive formative research to understand how seniors and people with disabilities learn
and make decisions about their Medi-Cal delivery options. Findings informed HRA’s development of a draft
consumer guidebook called “What Are My Medi-Cal Choices?” in English, Spanish, and Chinese. The
formative research used a participatory model where beneficiaries and other stakeholders were consulted in
the content and layout of the guidebook. HRA conducted 51 key informant interviews with stakeholders as
well as extensive qualitative research with Medi-Cal beneficiaries including 24 one-on-one interviews, 18
focus groups, and 36 one-on-one usability tests. This formative research was conducted in English, Spanish,
Mandarin, Cantonese, and American Sign Language. Formative research findings showed that that English-,
Spanish- and Chinese-speaking Medi-Cal recipients who are seniors or people with disabilities had very
little knowledge about their Medi-Cal choices and negative attitudes about managed care health plans.
Several areas of unmet information needs and primary areas of concern for SPD beneficiaries when faced
with Medi-Cal choices were also identified. In addition to the above formative research, an advisory group
that included disability advocates, managed care plan representatives, health care providers, policymakers,
and Medi-Cal beneficiaries provided guidance and feedback on the research, guidebook, the dissemination
process, and complementary interventions.
The Department of Health Care Services disseminated the guidebook through a direct mailing to
beneficiaries in the target population and via partner organizations. The final guidebook was developed in
12 threshold languages, plus alternative formats including Braille (English and Spanish only) and audio,
including MP3, cassette, and CD (all 12 languages).
HRA conducted a multi-lingual, mixed-methods evaluation of the final guidebook including 10 focus
groups, 28 stakeholder interviews, and a randomized control trial telephone survey. At six weeks post-
dissemination, the intervention group showed significantly higher increases in knowledge, confidence,
positive attitudes about, and intentions to consider changing to a Medi-Cal health plan than did the control
group. Overall, the findings provided strong evidence that the guidebook was an effective and low-cost way
to improve recipients’ abilities to make more informed Medi-Cal choices.
In 2008, the Institute for Healthcare Advancement jointly awarded HRA and the DHCS the national first place
award for Health Literacy for their work on the consumer guidebook.

Health Literacy Implications of the Affordable Care Act
21
III. Conclusion
he ACA is not a landmark piece of legislation for health literacy, but with its attention to increased
coverage, quality improvement and cost reduction, it creates opportunities for bringing cultural
competency, disparities, and health literacy to the fore. It establishes momentum for investments in
innovation among state agencies, payers, providers, regulators, advocacy groups, and others to improve
care in many ways, including patient-centered high quality care. Organizations promoting health literacy
will not be armed with forceful legislative or with regulatory mandates or with designated resources, so
they will have to continue to find ways to make the case for greater investment and action by both
public and private stakeholders in our health care system.
The ACA does create opportunities for driving home the importance of health literacy in all of the key
domains of health and health care identified earlier:
1. The Coverage Expansion: Establishing what is essentially universal coverage for 16 million
Americans up to 133 percent of FPL and subsidized insurance options for another 16 million low
income Americans will only be successful if the newly eligible individuals can understand their
options and navigate the enrollment process.
2. Equity: Moving toward universal coverage and creating the same “floor” for all of our lowest-
income populations should help address some of the fundamental disparities in access to care in
this country, but as the legislation underscores, that will depend on the attention our health care
delivery system pays to cultural differences, language, and by extension, literacy.
3. Workforce: The provider training provisions in ACA related to disparities, cultural competency,
and patient-centeredness all present opportunities for bringing greater attention to health
literacy.
4. Health care Information: From medication management to provider performance rating, patient
information must be presented at reading and numeracy levels accessible to millions of
Americans with low literacy skills.
5. Public Health and Wellness: The preparation and presentation (whether in print, electronically,
or otherwise) of consumer information on issues ranging from prevention to emergency
preparedness must be done with low literacy in mind.
6. Quality Improvement: The ACA’s emphasis on developing, testing and spreading best practices
for improving quality and reducing costs presents many new opportunities for making the case for
investments in health literacy.
T

Health Literacy Implications of the Affordable Care Act
22
IV. Appendices
*
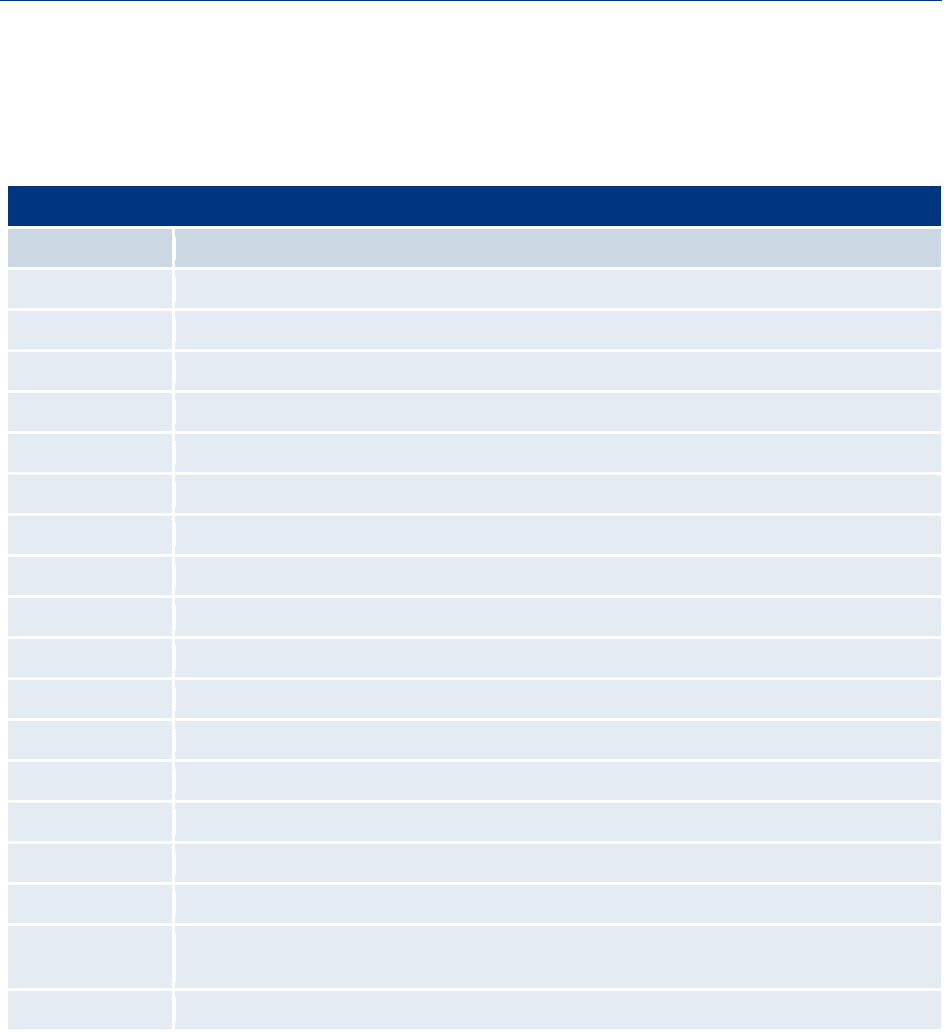
Appendix A: Summary of ACA Provisions with Potential Implications for Health
Literacy
Insurance Reform, Outreach, and Enrollment
Sec. 1002. Health insurance consumer information. The Secretary shall award grants to States to
enable them (or the Exchange) to establish, expand, or provide support for offices of health insurance
consumer assistance or health insurance ombudsman programs. These independent offices will assist
consumers with filing complaints and appeals, educate consumers on their rights and responsibilities, and
collect, track, and quantify consumer problems and inquiries.
Sec. 1103. Immediate information that allows consumers to identify affordable coverage options.
Establishes an Internet portal for beneficiaries to easily access affordable and four comprehensive
coverage options. This information will include eligibility, availability, premium rates, cost sharing, and
the percentage of total premium revenues spent on health care, rather than administrative expenses, by
the issuer. Section 10102 clarifies that the internet portal shall be available to small businesses and shall
contain information on coverage options available to small businesses.
Sec. 1311. Affordable choices of health benefit plans. Requires the Secretary to award grants, available
until 2015, to States for planning and establishment of American Health Benefit Exchanges. By 2014,
requires States to establish an American Health Benefit Exchange that facilitates the purchase of
qualified health plans and includes a SHOP Exchange for small businesses.
Sec. 1401. Refundable tax credit providing premium assistance for coverage under a qualified health
plan. Amends the Internal Revenue Code to provide tax credits to assist with the cost of health
insurance premiums.
Sec. 1413. Streamlining of procedures for enrollment through an Exchange and State Medicaid,
CHIP, and health subsidy programs. Requires the Secretary to establish a system for the residents of
each State to apply for enrollment in, receive a determination of eligibility for participation in, and
continue participation in, applicable State health subsidy programs. The system will ensure that if any
individual applying to an Exchange is found to be eligible for Medicaid or a State children’s health
insurance program (CHIP), the individual is enrolled for assistance under such plan or program.
Sec. 1513. Shared responsibility for employers. As amended by the Reconciliation Act, requires an
employer with at least 50 full-time employees that does not offer coverage and has at least one full-time
employee receiving a premium assistance tax credit to make a pay
ment of $2,000 per full-time employee.
Includes the number of full-time equivalent employees for purposes of determining whether an employer
has at least 50 employees. Exempts the first 30 full-time employees for the purposes of calculating the
amount of the payment. Section 10106 clarifies that the calculation of full-time workers is made on a
*
Adapted from the following:
• Communication with S. Rosenbaum (August – September 2010), Hirsh Professor and Chair of the Health Policy Department,
George Washington University.
• Democratic Policy Committee, U.S. Senate. Affordable Care Act: Section-by-Section Analysis with Changes Made by Title X
and Reconciliation. Updated September 17, 2010. Available at: http://dpc.senate.gov/dpcissue-.
• E. Williams and C. Redhead. Public Health Workforce, Quality, and Related Provisions in the Patient Protection and
Affordable Care Act (PPACA). Congressional Research Service (CRS) Report for Congress. 7-5700. June 2010. Available at:
http://www.crs.gov.

Health Literacy Implications of the Affordable Care Act
23
monthly basis. The Reconciliation Act eliminates the penalty for waiting periods before an employee may
enroll in coverage. An employer with at least 50 employees that does offer coverage but has at least one
full-time employee receiving the premium assistance tax credit will pay the lesser of $3,000 for each of
those employees receiving a tax credit or $2,000 for each of their full-time employees total, not including
the first 30 workers. The Secretary of Labor shall conduct a study to determine whether employees’ wages
are reduced by reason of the application of the assessable payments.
Sec. 2001. Medicaid coverage for the lowest income populations.
Creates a new State option to provide Medicaid coverage through a State plan amendment beginning on
April 1, 2010, as amended by Section 10201. Eligible individuals include: all non-elderly, non-pregnant
individuals who are not entitled to Medicare (e.g., childless adults and certain parents). Creates a new
mandatory Medicaid eligibility category for all such “newly-eligible” individuals with income at or below
133 percent of the FPL beginning January 1, 2014. As of January 1, 2014, the mandatory Medicaid
income eligibility level for children ages 6 to 19 changes from 100 percent to 133 percent FPL. Effective
April 1, 2010, states can provide Medicaid coverage to all non-elderly individuals above 133 percent of
FPL through a State plan amendment.
Sec. 2715. Development and utilization of uniform explanation of coverage documents and
standardized definitions. Requires the Secretary to develop standards for use by health insurers in
compiling and providing an accurate summary of benefits and explanation of coverage for applicants,
policyholders or certificate holders, and enrollees. Standards must be in a uniform format, using language
that is easily understood by the average enrollee, and must include uniform definitions of standard
insurance and medical terms. The explanation must also describe any cost-sharing, exceptions,
reductions, and limitations on coverage, and examples of common benefits scenarios.
Sec. 3306. Funding outreach and assistance for low-income programs. Provides $45 million for
outreach and education activities to State Health Insurance Programs, Administration on Aging, Aging
Disability Resource Centers and the National Benefits Outreach and Enrollment.
Sec. 5000A. Requirement to maintain minimum essential coverage. Requires individuals to maintain
minimum essential coverage beginning in 2014. As amended by Section 1002 of the Reconciliation Act,
failure to do so will result in a penalties, with exceptions and exemptions.
Individual Protections, Equity and Special Populations
Sec. 1557. Nondiscrimination. Protects individuals against discrimination under the Civil Rights Act,
the Education Amendments Act, the Age Discrimination Act, and the Rehabilitation Act, through
exclusion from participation in or denial of benefits under any health program or activity.
Sec. 2405. Funding to expand State Aging and Disability Resource Centers. Appropriates, to the
Secretary of HHS, $10 million for each of FY 2010 - 2014 to carry out Aging and Disability Resource
Center (ADRC) initiatives.
Sec. 4302. Understanding health disparities; data collection and analysis. Ensures that any ongoing or
new Federal health program achieve the collection and reporting of data by race, ethnicity, primary
language and any other indicator of disparity.

Health Literacy Implications of the Affordable Care Act
24
Sec. 6105. Standardized complaint form. Requires the Secretary to develop a standardized complaint
form for use by nursing home residents (or a person acting on a resident’s behalf) in filing complaints
with a State survey and certification agency and a State long-term care ombudsman program. States
would also be required to establish complaint resolution processes.
Sec. 6121. Dementia and abuse prevention training. Requires facilities to include dementia
management and abuse prevention training in pre-employment initial training for permanent and
contract or agency staff, and if the Secretary determines appropriate, in ongoing in-service training.
Sec. 6301. Patient-Centered Outcomes Research. Establishes a private, nonprofit entity (the Patient-
Centered Outcomes Research Institute) governed by a public-private sector board to identify priorities
for and provide for the conduct of comparative outcomes research. Requires the Institute to ensure that
subpopulations are appropriately accounted for in research designs.
Sec. 6703. Elder Justice. Requires the Secretary of HHS, in consultation with the Departments of
Justice and Labor, to award grants and carry out activities that provide greater protection to those
individuals seeking care in facilities that provide long-term services and supports and provide greater
incentives for individuals to train and seek employment at such facilities.
Sec. 10212. Pregnancy Assistance Fund. Establishes a Pregnancy Assistance Fund for the purpose of
awarding competitive grants to States to assist pregnant and parenting teens and women. The grants will
help fund a seamless network of supportive services to help pregnant and parenting teens and women
complete high school or postsecondary degrees, and gain access to health care, child care, family housing,
and other critical supports. In addition, funding recipients will be encouraged to address violence against
pregnant and parenting women.
Sec. 10221. Indian health care improvement. Authorizes appropriations for the Indian Health Care
Improvement Act, including programs to increase the Indian health care workforce, new programs for
innovative care delivery models, behavioral health care services, new services for health promotion and
disease prevention, and efforts to improve access to health care services.
Sec. 10334. Minority health. Codifies the Office of Minority Health at HHS and a network of minority
health offices located within HHS. Elevates the National Center on Minority Health and Health
Disparities at the National Institutes of Health from a Center to an Institute. The Offices of Minority
Health will monitor health, health care trends, and quality of care among minority patients and evaluate
the success of minority health programs and initiatives.
Workforce Development
Sec. 5203. Health care workforce loan repayment programs. Establishes a loan repayment program for
pediatric subspecialists and providers of mental and behavioral health services to children and
adolescents who are or will be working in a Health Professional Shortage Area, Medically Underserved
Area, or with a Medically Underserved Population.
Sec. 5205. Allied health workforce recruitment and retention program. Offers loan repayment to
allied health professionals employed at public health agencies or in settings providing health care to
patients in settings located in Health Professional Shortage Areas, Medically Underserved Areas, or
serving Medically Underserved Populations.

Health Literacy Implications of the Affordable Care Act
25
Sec. 5301. Training in family medicine, general internal medicine, general pediatrics, and physician
assistantship. Provides grants to develop and operate training programs, to provide financial assistance
to trainees and faculty, to enhance faculty development in primary care and physician assistant programs,
and to establish, maintain, and improve academic units in primary
care. Priority is given to programs
that educate students in team-based approaches to care, including the patient-centered medical
home.
Sec. 5305. Geriatric education and training; career awards; comprehensive geriatric education.
Authorizes funding to geriatric education centers to support training in geriatrics, chronic care
management, and long-term care for faculty in health professions schools and family caregivers; develop
curricula and best practices in geriatrics; expand the geriatric career awards to advanced practice nurses,
clinical social workers, pharmacists, and psychologists; and establish traineeships for individuals who are
preparing for advanced education nursing degrees in geriatric nursing.
Sec. 5307. Cultural competency, prevention, and public health and individuals with disabilities
training. Reauthorizes and expands programs to support the development, evaluation, and dissemination
of model curricula for cultural competency, prevention, and public health proficiency and aptitude for
working with individuals with disabilities training for use in health professions schools and continuing
education programs.
Sec. 5309. Nurse education, practice, and retention grants. Awards grants to nursing schools to
strengthen nurse education and training programs and to improve nurse retention.
Sec. 5313. Grants to promote the community health workforce. Authorizes the Secretary to award
grants to States, public health departments, clinics, hospitals, Federally Qualified Health Centers
(FQHCs), and other nonprofits to promote positive health behaviors and outcomes in medically
underserved areas through the use of community health workers. Community health workers offer
interpretation and translation services, provide culturally appropriate health education and information,
offer informal counseling and guidance on health behaviors, advocate for individual and community
health needs, and provide some direct primary care services and screenings.
Sec. 5316. Rural physician training grants. As added by Section 10501, establishes a grant program for
medical schools to recruit and train medical students to practice medicine in underserved rural
communities.
Sec. 5317. Demonstration grants for family nurse practitioner training programs. As added by
Section 10501, establishes a training demonstration program that supports recent Family Nurse
Practitioner graduates in primary care for a 12-month period in FQHCs and nurse-managed health
clinics. The demonstration is authorized from 2011 through 2014
Sec. 5401. Centers of excellence. The Centers of Excellence program, which develops a minority
applicant pool to enhance recruitment, training, academic performance and other supports for minorities
interested in careers in health, is reauthorized.
Sec. 5402. Health professions training for diversity. Provides scholarships for disadvantaged students
who commit to work in medically underserved areas as primary care providers, and expands loan
repayments for individuals who will serve as faculty in eligible institutions.

Health Literacy Implications of the Affordable Care Act
26
Sec. 5403. Interdisciplinary, community-based linkages. Authorizes funding to establish community-
based training and education grants for Area Health Education Centers and Programs. Supports two
programs targeting individuals from urban and rural medically underserved communities, who are seeking
careers in the health professions.
Sec. 5507. Demonstration project to address health professions workforce needs; extension of
family-to-family health information centers. Establishes a demonstration grant program through
competitive grants to provide aid and supportive services to low-income individuals with the opportunity
to obtain education and training for occupations in the health care field that pay well and are expected
to experience labor shortages or be in high demand. The demonstration grant is to serve low-income
persons including recipients of assistance under State Temporary Assistance for Needy Families (TANF)
programs.
Sec. 5602. Negotiated rulemaking for development of methodology and criteria for designating
medically underserved populations and health professions shortage areas. Directs the Secretary, in
consultation with stakeholders, to establish a comprehensive methodology and criteria for designating
medically underserved populations and Health Professional Shortage Areas.
Sec. 5606. State grants to health care providers who provide services to a high percentage of
medically underserved populations or other special populations. As added by Section 10501, creates a
grant program to support health care providers who treat a high percentage of medically underserved
populations.
Sec 9024. Health professionals State loan repayment tax relief. As added by Section 10908, excludes
from gross income payments made under any State loan repayment or loan forgiveness program that is
intended to provide for the increased availability of health care services in underserved or health
professional shortage areas.
Health Information
Sec. 3305. Improved information for subsidy-eligible individuals reassigned to prescription drug
plans and MA–PD plans. Requires HHS, beginning in 2011, to transmit formulary and coverage
determination information to subsidy-eligible beneficiaries who have been automatically reassigned to a
new Part D low-income subsidy plan.
Sec. 3503. Grants to implement medication management services in treatment of chronic disease.
Creates a program to support medication management services by local health providers.
Sec. 3507. Presentation of prescription drug benefit and risk information. Requires the Food and
Drug Administration to evaluate and determine if the use of drug fact boxes which would clearly
communicate drug risks and benefits and support clinician and patient decision making in advertising
and other forms of communication for prescription medications is warranted.
Sec. 4205. Nutrition labeling of standard menu items at chain restaurants. Stipulates that a restaurant
that is part of a chain with 20 or more locations doing business under the same name are required to
disclose calories on the menu board and in a written form, as well as provide customers with additional
nutritional information upon request.

Health Literacy Implications of the Affordable Care Act
27
Sec. 10328. Improvement in Part D medication therapy management programs. Requires Part D
prescription drug plans to include a comprehensive review of medications and a written summary of the
review as part of their medication therapy management programs.
Public Health, Health Promotion, and Prevention & Wellness
Sec. 2951. Maternal, infant, and early childhood home visiting programs. Provides funding to States,
tribes, and territories to develop and implement one or more evidence-based Maternal, Infant, and Early
Childhood Visitation model(s). Models aimed at reducing infant and maternal mortality and its related
causes.
Sec. 2953. Personal responsibility education. Provides $75 million per year through FY2014 for
Personal Responsibility Education grants to States for programs to educate adolescents on both
abstinence and contraception for prevention of teenage pregnancy and sexually transmitted infections,
including HIV/AIDS. Funding is also available for 1) innovative teen pregnancy prevention strategies
and services to high-risk, vulnerable, and culturally under-represented populations, 2) allotments to
Indian tribes and tribal organizations, and 3) research and evaluation,
training, and technical
assistance.
Sec. 4001. National Prevention, Health Promotion and Public Health Council. Creates an
interagency council dedicated to promoting healthy policies at the federal level. The Council will
establish a national prevention and health promotion strategy and develop interagency working
relationships to implement the strategy.
Sec. 4002. Prevention and Public Health Fund. Establishes a Fund to provide an expanded and
sustained national investment in prevention and public health programs to improve health and help
restrain the rate of growth in private and public sector health care costs.
Sec. 4003. Clinical and community preventive services. Expands the efforts of, and improves the
coordination between the U.S. Preventive Services Task Force and the Community Preventive Services
Task Force. The latter uses a public health perspective to review the evidence of effectiveness of
population-based preventive services such as tobacco cessation, increasing physical activity and
preventing skin cancer, and develops recommendations for their use.
Sec. 4004. Education and outreach campaign regarding preventive benefits. Directs the Secretary to
convene a national public/private partnership for the purposes of conducting a national prevention and
health promotion outreach and education campaign. The goal of the campaign is to raise awareness of
activities to promote health and prevent disease across the lifespan. The Secretary will conduct a
national media campaign on health promotion and disease prevention focusing on nutrition, physical
activity, and smoking cessation using science-based social research. The Secretary shall also maintain a
web-based portal that provides informational guidelines on health promotion and disease prevention to
health care providers and the public as well as a personalized prevention plan tool for individuals to
determine their disease risks and obtain tailored guidance on health promotion and disease prevention.
In addition, the Secretary will provide guidance and relevant information to States and health care
providers regarding preventive and obesity-related services that are available to Medicaid enrollees.
Each State will be required to design a public awareness campaign to educate Medicaid enrollees
regarding availability and coverage of such services.
Sec. 4102. Oral healthcare prevention activities. Establishes an oral healthcare prevention education
campaign at the CDC, focusing on prevention and targeting populations including children and

Health Literacy Implications of the Affordable Care Act
28
pregnant women. Creates demonstration programs on oral health care delivery and strengthens
surveillance capacity.
Sec. 4103. Medicare coverage of annual wellness visit providing a personalized prevention plan.
Provides coverage under Medicare, with no co-payment or deductible, for an annual wellness visit and
personalized prevention plan services.
Sec. 4107. Coverage of comprehensive tobacco cessation services for pregnant women in Medicaid.
States would be required to provide Medicaid coverage for counseling and pharmacotherapy to pregnant
women for cessation of tobacco use
Sec. 4108. Incentives for prevention of chronic diseases in Medicaid. The Secretary would award
grants to States to provide incentives for Medicaid beneficiaries to participate in programs promoting
healthy lifestyles.
Sec. 4201. Community transformation grants. Authorizes the Secretary to award competitive grants to
eligible entities for programs that promote individual and community health and prevent incidence of
chronic disease.
Sec. 4202. Healthy aging, living well; evaluation of community-based prevention and wellness
programs for Medicare beneficiaries. The goal of this program is to improve the health status of the pre-
Medicare-eligible population to help control chronic disease and reduce Medicare costs. The CDC will
provide grants to States or large local health departments to conduct pilot programs in the 55-to-64 year
old population. Pilot programs would evaluate chronic disease risk factors, conduct evidence-based public
health interventions, and ensure that individuals identified with chronic disease or at-risk for chronic
disease receive clinical treatment to reduce risk. Pilot programs will be evaluated for success in
controlling Medicare costs in the community. Additionally, the Centers for Medicare & Medicaid
Services (CMS) will conduct a comprehensive assessment of community-based disease self-management
programs that help control chronic diseases. The Secretary will then
develop a plan for improving
access to such services for Medicare beneficiaries.
Sec. 4206. Demonstration project concerning individualized wellness plan. This pilot program
provides at-risk populations who utilize community health centers with a comprehensive risk-factor
assessment and individualized wellness plan to reduce risk factors for preventable conditions.
Sec. 4301. Research on optimizing the delivery of public health services. The Secretary, through the
Director of CDC, shall provide funding for research in the area of public health services and systems.
Research shall examine best practices relating to prevention, analyze the translation of interventions
from academic institutions to clinics and communities, and identify effective strategies for delivering
public health services in real-world settings.
Sec. 4303. CDC and employer-based wellness programs. Requires the CDC to study and evaluate best
employer-based wellness practices and provide an educational campaign and technical assistance to
promote the benefits of worksite health promotion to employers.
Sec. 4306. Funding for childhood obesity demonstration project. Appropriates $25 million for a
demonstration project to develop a comprehensive and systematic model for reducing childhood obesity,
which the Secretary must initiate under the Children's Health Insurance Program Reauthorization Act
of 2009.

Health Literacy Implications of the Affordable Care Act
29
Sec. 10408. Grants for small businesses to provide comprehensive workplace wellness programs.
Authorizes an appropriation of $200 million to give employees of small businesses access to
comprehensive workplace wellness programs.
Sec. 10413. Young women’s breast health awareness and support of young women diagnosed with
breast cancer. Directs the Secretary of HHS to develop a national education campaign for young women
and health care professionals about breast health and risk factors for breast cancer. Supports prevention
research activities at the Centers for Disease Control and Prevention (CDC) on breast cancer in younger
women.
Sec. 10501. National diabetes prevention program. Establishes a national diabetes prevention program
at the CDC. State, local, and tribal public health departments and non-profit entities can use funds for
community-based prevention activities, training and outreach, and evaluation.
Innovations in Quality and the Delivery and Costs of Care
Sec. 2703. State option to provide health homes for enrollees with chronic conditions. Provides
States the option of enrolling Medicaid beneficiaries with chronic conditions into a health home. Health
homes would be composed of a team of health professionals and would provide a comprehensive set of
medical services, including care coordination.
Sec. 3011. National strategy. Requires the Secretary to establish and update annually a national
strategy to improve the delivery of health care services, patient health outcomes, and population health.
Establishes, not later than January 1, 2011, a federal health care quality internet website.
Sec. 3012. Interagency working group on health care quality. Requires the President to convene a
working group comprising federal agencies to collaborate on the development and dissemination of
quality initiatives consistent with the national strategy.
Sec. 3013. Quality measure development. Authorizes $75 million over five years for the development
of quality measures at Agency for Healthcare Research and Quality (AHRQ) and the Centers for
Medicare and Medicaid Services (CMS). Measures must be consistent with the national strategy. As
amended by Section 10303, requires the Secretary to develop and publicly report on patient outcomes
measures.
Sec. 3014. Quality measurement. Provides $20 million to support the endorsement and use of endorsed
quality and efficiency measures by the HHS Secretary for use in Medicare, reporting performance
information to the public, and in health care programs.
Sec. 3015. Data Collection; Public Reporting. Requires the Secretary to collect and aggregate
consistent data on quality and resource use measures from information systems used to support health
care delivery to implement the public reporting of performance information.
Sec. 3021. Establishment of Center for Medicare and Medicaid Innovation within CMS. The purpose
of the Center will be to research, develop, test, and expand innovative payment and delivery
arrangements to improve the quality and reduce the cost of care provided to patients in each program.
Sec. 3501. Health care delivery system research; Quality improvement technical assistance. Builds on
AHRQ’s Center for Quality Improvement and Patient Safety to support research, technical assistance

Health Literacy Implications of the Affordable Care Act
30
and process implementation grants. Grants funded will identify, develop, evaluate, disseminate, and
provide training in innovative methodologies and strategies for quality improvement practices in the
delivery of health care services.
Sec. 3502. Grants or contracts to establish community health teams to support the patient-centered
medical home. Creates a program to establish and fund the development of community health teams to
support the development of medical homes by increasing access to comprehensive, community based,
coordinated care.
Sec. 3506. Program to facilitate shared decision-making. Establishes a program at HHS for the
development, testing, and disseminating of educational tools to help patients, caregivers, and authorized
representatives understand their treatment options.
Sec. 3510. Patient navigator program. Reauthorizes demonstration programs to provide patient
navigator services within communities to assist patients overcome barriers to health services.
Sec. 10330. Modernizing computer and data systems of CMS to support improvements in care
delivery. Requires the Secretary of HHS to develop a plan to modernize the computer and data systems
of CMS to support improvements in care delivery.
Sec. 10331. Public reporting of performance information. Requires the Secretary of HHS to develop a
“Physician Compare” website where Medicare beneficiaries can compare scientifically sound measures of
physician quality and patient experience measures.
Sec. 10333. Community-based collaborative care networks. Provides grants to develop networks of
providers to deliver coordinated care to low-income populations.
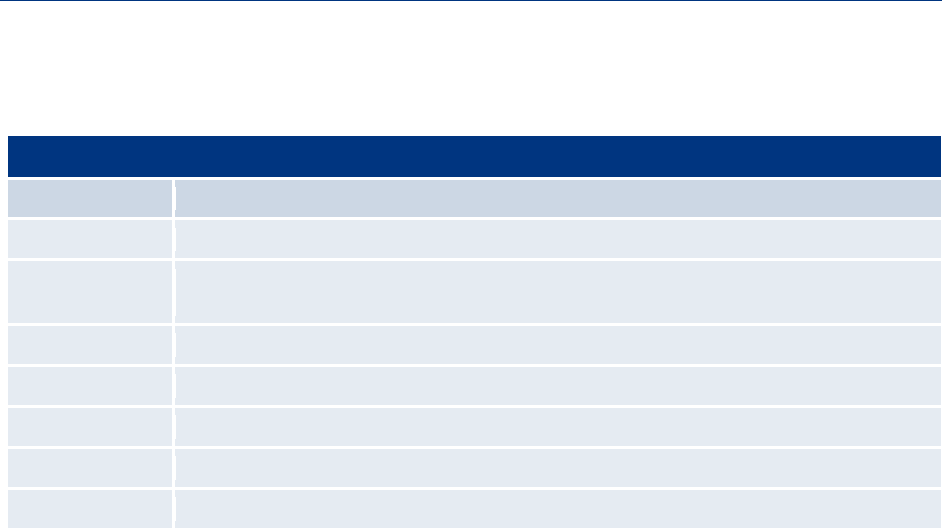
Health Literacy Implications of the Affordable Care Act
31
Appendix B: Instances of “Culturally and Linguistically Appropriate” in the ACA
Culturally and Linguistically Appropriate
Section Number Provision Title
Sec. 1311 Affordable choices of health benefit plans.
Sec. 2715 Development and utilization of uniform explanation of coverage documents and standardized
definitions.
Sec. 2719 Appeals process.
Sec. 4102 Oral healthcare prevention activities.
Sec. 5313 Grants to promote the community health workforce.
Sec. 5405 Primary care extension program.
Sec. 10410 Centers of excellence for depression
